| Share |  |
 | |||
Controlling Insulin--The Best Way To Guard Your Health And Lose Weight
 Maintaining good blood sugar control and insulin levels is one of the most important ways to protect yourself from an array of symptoms and health conditions that can diminish your quality of life and, in many instances, shorten your lifespan. Keeping low levels of the hormone responsible for turning calories into fat can also help you win the struggle against those extra pounds that tend to accumulate with age.
Maintaining good blood sugar control and insulin levels is one of the most important ways to protect yourself from an array of symptoms and health conditions that can diminish your quality of life and, in many instances, shorten your lifespan. Keeping low levels of the hormone responsible for turning calories into fat can also help you win the struggle against those extra pounds that tend to accumulate with age.
Most people are unaware of their insulin levels unless they should discover they are diabetic. After all, insulin screening is typically not included in conventional blood work as is fasting glucose levels. While people may realize that diabetics can experience increased risk of complications (heart attack, stroke, high blood pressure, obesity, amputations, blindness, kidney failure, nerve damage, impotence, dementia and certain cancers), very few understand that decades before blood sugar levels even start to climb, a condition known as insulin resistance promotes rising insulin levels that significantly increase the risk for those and other serious health issues.
Early Awareness – the Wiser Path
Dr. Mark Hyman, the author of the “The Blood Sugar Solution”, reveals that by the time a person is diagnosed with diabetes, insulin and blood sugar imbalances have been in play that could have been detected decades years earlier. Scientists estimate that by the year 2020, one out of two people will be 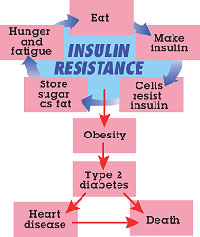 affected by a continuum of health problems that range from mild insulin resistance and excess weight to obesity and diabetes. And even more sobering is the fact that 90% of them will likely go undiagnosed.
affected by a continuum of health problems that range from mild insulin resistance and excess weight to obesity and diabetes. And even more sobering is the fact that 90% of them will likely go undiagnosed.
How much wiser to recognize imbalances before they turn into long-term health problems and induce damage that, in some cases, is irreversible. Insulin resistance sets the stage for pre-diabetes and people with pre-diabetes usually are classified as type 2 diabetics within 10 years unless they make significant dietary and lifestyles changes to reverse the progression.
Although no clearly defined symptoms for insulin resistance exist, a number of early warning signs indicate the likelihood of its occurrence and that blood sugar may be out of balance. Fatigue or sleepiness after meals, sugar cravings, constant hunger, weight gain, inability to lose weight, hormone imbalance, and poor concentration or fuzzy thinking can take place when your body is struggling to process the energy in food and maintain proper blood sugar balance.
Understanding Insulin Resistance – the Best Means of Prevention
The best way to prevent (or reverse) a condition is to understand how it developed in the first place. Since insulin resistance is a root cause of so many commonly experienced health conditions, gaining a fundamental understanding of what it is and how it progresses is essential.
Insulin is a hormone secreted by special cells in the pancreas (beta cells) in response to glucose levels that rise in the blood primarily when carbohydrates are digested and absorbed. Insulin’s main job is to facilitate the moving of glucose and other nutrients from the bloodstream into cells where they are transformed into energy to meet the body’s needs. Glucose that is not immediately needed to fuel muscle cells is sent to the liver and converted to a storage form of fuel called glycogen (should blood sugar levels get too low, glucagon, an opposing hormone to insulin, converts glycogen back into usable energy).
When limited glycogen stores are maxed out, the liver converts excess glucose to cholesterol and triglycerides (fatty acids) and the rest is stored in fat cells. Since the body needs only about a teaspoon of glucose at any given time to meet its needs, it endeavors to put the excess into storage sites due to how damaging it is to the body.
This energy delivery and storage hormone works by binding with insulin receptors located on the surface of cells that act like a one-way door to allow the inflow of blood sugar. Insulin signals special protein transporters inside the cell to rise to the cell membrane surface where they latch onto glucose molecules 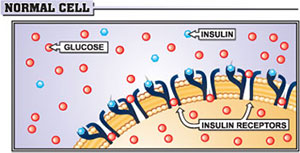 and draw them inside. Once insulin “unlocks” the door to facilitate the entry of glucose into cells, blood levels return to a normal range and the pancreas stops secreting it until the next time food is consumed. Only a minimum release of insulin is required to effectively and efficiently clear glucose from the blood in normal, healthy cells sensitive to the message insulin sends.
and draw them inside. Once insulin “unlocks” the door to facilitate the entry of glucose into cells, blood levels return to a normal range and the pancreas stops secreting it until the next time food is consumed. Only a minimum release of insulin is required to effectively and efficiently clear glucose from the blood in normal, healthy cells sensitive to the message insulin sends.
The condition of insulin resistance begins when surges of insulin are repeatedly triggered by ongoing exposure to high levels of glucose in the blood that occur when sugar-laden, refined and processed carbohydrates are eaten on a regular basis. These types of simple carbs (sugars, breads, cereal grains, pasta, products made from flour or foods high in starch like white rice and potatoes) break down almost instantly to glucose molecules and cause blood sugar levels to rise sharply.
Not all carbohydrates affect blood sugar so dramatically. Whole food forms of complex carbohydrates (non-starchy vegetables, legumes, nuts, seeds, beans, and low-glycemic fruits) impact blood sugar levels to a much lesser degree due to the higher amounts of fiber and other nutrients they contain that serve to slow down carbohydrate digestion and absorption.
The main reason it is so important to avoid blood sugar spikes is that they cause the pancreas to overreact and produce unnaturally high amounts of insulin in order to more quickly clear glucose from the bloodstream. But often when too much insulin is pumped out at one time, blood sugar levels drop too low  and result in a “crash”, or loss of energy that can make a person feel extra tired, cranky, foggy, and sometimes even light-headed or shaky. The body naturally craves another “hit”, which typically leads to eating more of the wrong type of carbohydrates. This shoots glucose levels back up, creating an up and down blood sugar “roller coaster” effect.
and result in a “crash”, or loss of energy that can make a person feel extra tired, cranky, foggy, and sometimes even light-headed or shaky. The body naturally craves another “hit”, which typically leads to eating more of the wrong type of carbohydrates. This shoots glucose levels back up, creating an up and down blood sugar “roller coaster” effect.
How Does Insulin Resistance Develop?
Insulin receptors constantly exposed to insulin trying to get more glucose inside become oversaturated and less and less responsive to the “noise” of its persistent signals. Since cells only handle so much energy input at a time, they begin to resist efforts to overfill them. Communication breaks down between insulin and cell receptors to the point where cells basically tune insulin out and pay little attention to its message to store more fuel since “enough is enough”. When cell receptors become desensitized to insulin and cease to function normally, increased amounts are needed to usher glucose into the cell. This is insulin resistance.
The fact that insulin can no longer successfully accomplish its mission causes the pancreas to go into overdrive and accelerate its output in order to keep damaging high levels of glucose out of the blood. In the early stages, glucose levels eventually normalize but once insulin resistance sets in more, it can take five 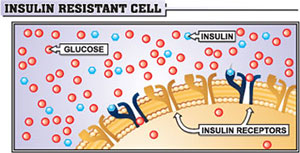 times the normal amount to lower them. The higher insulin levels rise, the harder the body has to work to keep glucose levels down, especially when high carbohydrate foods are eaten. Meanwhile, continually “force-feeding” cells already overwhelmed with processing too much glucose creates damaging oxidative stress and subsequent free radical activity that is detrimental to the body.
times the normal amount to lower them. The higher insulin levels rise, the harder the body has to work to keep glucose levels down, especially when high carbohydrate foods are eaten. Meanwhile, continually “force-feeding” cells already overwhelmed with processing too much glucose creates damaging oxidative stress and subsequent free radical activity that is detrimental to the body.
Fasting glucose levels may still be within normal ranges at this point but the problem is that insulin levels are staying elevated for longer and longer periods of time. Insulin’s inflammatory effects begin to take their toll throughout the body. As time goes on and cells become even more resistant, no amount of insulin can do the job. At this point, blood sugar levels that were only elevated too high after meals begin to stay elevated even at fasting levels.
Eventually the condition of insulin resistance causes the insulin-producing cells in the pancreas to wear out from staying in overdrive so long. Type 2 diabetes is basically full blown insulin resistance. The irony is that the very cells that were designed to keep blood sugar under control are themselves destroyed from the toxic effects of chronically high levels of glucose.
Save Your Health by Managing Your Insulin Levels
Keeping your cells sensitive to insulin is probably the most important way to stay healthy and prevent many of the disease conditions on the rise today. The body can be no healthier than its cells which depend on the energy produced from glucose to fuel its processes. Cells cannot access adequate amounts of glucose when insulin resistance reaches a certain point. And since insulin is known as the “master hormone”, cells that are unresponsive to the message of insulin also fail to respond properly to the message of other hormones.
You can effectively control your health and slow the rate of aging and deterioration by controlling your blood sugar and insulin levels.
 Neither glucose nor insulin was meant to stay in the bloodstream in higher amounts for any length of time. Inflammatory and corrosive effects can occur in the body when they do and inflammation is at the root of most chronic degenerative diseases.
Neither glucose nor insulin was meant to stay in the bloodstream in higher amounts for any length of time. Inflammatory and corrosive effects can occur in the body when they do and inflammation is at the root of most chronic degenerative diseases.
For instance, glucose that remains high in the blood for any period of time causes a chemical reaction known as glycation in which glucose molecules chemically react with and damage proteins in the body, destroying their ability to function properly (enzymes and hormones are examples of proteins). These “Advanced Glycation End-products” or AGEs, as they are called, build up in cells, damage tissue and can lead to complications of the nerves and eyes such as cataracts and peripheral neuropathy. They are also thought to be responsible for many of the effects of aging such as wrinkles.
Conditions Linked with Insulin Resistance
Insulin resistance is a central underlying root cause of numerous interrelated health problems. Described below are some of the symptoms and conditions associated with and/or caused by insulin resistance.
 Type 2 Diabetes
Type 2 Diabetes
Insulin resistance alone does not cause type 2 diabetes but the high demand it places on the insulin-producing beta cells sets the stage for the disease. When insulin levels go high, the risk is increased eight-fold. High blood sugar levels also damage insulin-producing cells. When blood sugar levels rise even slightly above 100 for as little as two hours, failure of the beta cells in the pancreas is detectable. Even with blood sugar levels as low as 110; people can lose as much as 40% of their beta cell capacity in as little as two years. The higher the blood sugar, the more damage to the beta cells occurs and these are never replaced.
Excess Weight and “Belly Fat”
 Being overweight dramatically increases the risk of insulin resistance and insulin resistance causes further weight gain, obesity (being 30 pounds or more over ideal weight) and the development of abdominal or “belly” fat that puts a person at high risk for inflammation-based diseases (heart disease, diabetes, cancer, etc.). Insulin not only converts excess glucose to fat but it also shifts the body into fat-storing mode. Stored fat does not get released by glucagon to be burned for energy when insulin levels remain elevated due to an overabundance of glucose. The presence of insulin in the bloodstream makes it next to impossible to burn excess stored fat and forces the body to burn carbohydrates for energy instead. When cells become resistant to insulin, they become resistant as well to the signals of other hormones involved in weight control such as leptin that tells the brain when you need to stop eating and ghrelin that controls hunger.
Being overweight dramatically increases the risk of insulin resistance and insulin resistance causes further weight gain, obesity (being 30 pounds or more over ideal weight) and the development of abdominal or “belly” fat that puts a person at high risk for inflammation-based diseases (heart disease, diabetes, cancer, etc.). Insulin not only converts excess glucose to fat but it also shifts the body into fat-storing mode. Stored fat does not get released by glucagon to be burned for energy when insulin levels remain elevated due to an overabundance of glucose. The presence of insulin in the bloodstream makes it next to impossible to burn excess stored fat and forces the body to burn carbohydrates for energy instead. When cells become resistant to insulin, they become resistant as well to the signals of other hormones involved in weight control such as leptin that tells the brain when you need to stop eating and ghrelin that controls hunger.
Cardiovascular Disease
Cardiovascular disease is the leading cause of death in both men and women. In those with insulin resistance that progresses to diabetes, three-fourths will ultimately die of heart disease. Insulin resistance takes a toll on the cardiovascular system long before it becomes clinically evident, damaging blood vessels and altering blood lipid levels (elevated LDL, VLDL and triglycerides and lowered HDL). Rather than dietary fat, the real cause of these abnormal blood fat levels stem from excess carbohydrate consumption that leads to elevated levels of insulin and glucose in conjunction with insulin resistance. In his book “Reversing Diabetes”, Dr. Julian Whitaker states that insulin resistance is as accurate a predictor of heart disease as elevated LDL and may account for half of all heart attacks”.
The inflammatory damage produced in the lining of arteries is thought to be caused by the oxidation of small, dense LDL particles that squeeze between layers of cells and become stuck in the artery lining. Plaque formation that occurs when these wedged small dense particles oxidize and turn rancid prompts the 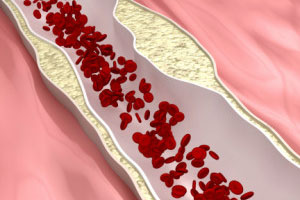 liver to produce even more LDL cholesterol to repair the damage. You should be aware that LDL numbers alone do not necessarily equate with arterial damage and increased risk of heart disease as it depends upon the type of LDL based on particle size (a blood test called the NMR LipoProfile test is designed to identify and quantify LDL particles as to their size and number and should be requested if your LDL levels are high in order to assess your true risk).
liver to produce even more LDL cholesterol to repair the damage. You should be aware that LDL numbers alone do not necessarily equate with arterial damage and increased risk of heart disease as it depends upon the type of LDL based on particle size (a blood test called the NMR LipoProfile test is designed to identify and quantify LDL particles as to their size and number and should be requested if your LDL levels are high in order to assess your true risk).
Insulin resistance and high glucose levels from eating too many refined carbohydrates induce the liver to manufacture greater amounts of triglycerides to store excess fat created by insulin from the overload of glucose. Since low-density lipoproteins (LDL) contain little protein and are mainly carriers of fat, greater amounts of that type are generated when triglyceride levels are high. Another way increased triglycerides promote heart disease is that they are deposited around the midsection in the form of visceral or “belly” fat, a dangerous form of fat that churns out hormones and inflammatory molecules and is a direct risk factor for heart disease, stroke, atherosclerosis, high blood pressure, cancer and kidney disease.
High insulin raises levels of fibrinogen, a substance that encourages the formation of blood clots and contributes to high blood pressure levels. High insulin also contributes to processes involved in inflammation that thickens blood and makes it stickier in addition to making blood vessels less elastic and able to respond to changes in pressure. Damage that occurs to blood vessels from high blood pressure results in decreased blood flow to vital organs, especially the heart (unfortunately, controlling high blood pressure with medication does nothing to stop this damage).
All of the above factors contribute to arteriosclerosis, a progressive thickening and hardening of arteries responsible for coronary artery disease, strokes and peripheral vascular disease.
Alzheimer’s, Dementia and Other Cognitive Disorders
Studies and research in recent years point to a connection between insulin resistance (particularly in those with type 2 diabetes), and accelerated brain plaque development associated with Alzheimer’s disease. A 2004 study revealed that people with diabetes can have as much as a 65 percent higher risk of developing Alzheimer’s. Studies also indicate a significantly higher risk for predementia and MCI (Mild Cognitive Impairment) in individuals with higher blood glucose levels. A type of insulin resistance in the brain is thought to affect normal brain signals and transmission of brain chemicals.
Other Conditions
- Fatty liver – accumulation of fat in the liver that is a manifestation of disordered control of lipids (blood fats).
- Gout and kidney stones – high insulin levels interfere with the kidney’s ability to clear uric acid from the body.
- Cancer – insulin stimulates unregulated cell growth and gene activation. Liver, pancreatic, endometrial, breast, prostate and colon cancer are the forms most commonly linked with insulin resistance.
- Polycystic ovarian syndrome (PCOS) – this hormone imbalance syndrome is clearly connected with insulin resistance and at least 40% of women who have it will have pre-diabetes or type 2 diabetes by the time they are 40 years of age.
- Kidney, eye and nerve damage – glucose builds up in capillaries and reduces blood flow to these areas.
- Infections – impaired circulation and damaged nerves increase the risk of infection and slow wound healing time.
- Fatigue – glucose cannot sufficiently get into the cell to produce energy.
Symptoms and Risk Factors of Insulin Resistance
 In many cases, the risk factors and symptoms are one and the same. If any of the following symptoms, conditions or lifestyle factors apply to you, it is possible that you may already have some degree of insulin resistance or may be more susceptible to developing it.
In many cases, the risk factors and symptoms are one and the same. If any of the following symptoms, conditions or lifestyle factors apply to you, it is possible that you may already have some degree of insulin resistance or may be more susceptible to developing it.
- Extra “belly fat” and/or excess weight - since fat deactivates insulin and raises blood glucose, the more overweight a person is, the more resistant to insulin they become. A gain of just 11-16 pounds doubles the risk of type 2 diabetes, while a gain of 17-24 pounds triples the risk. Severely overweight individuals demand as much as ten times greater amounts of insulin than people of normal weight require. Even if the insulin-producing capacity of an overweight person can handle the higher demands without becoming diabetic, higher insulin levels still place them at much greater risk for heart disease.
- Inability to Lose Weight – stubborn weight can result from cells starving due to lack of efficient absorption of glucose coupled with the fact that the body tends to hold on tightly to existing stores of energy when it perceives a shortage in fuel. What glucose the body does absorb goes straight into fat storage.
- BMI (Body Mass Index) - over 25
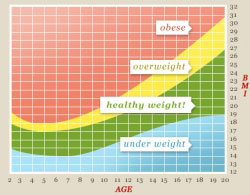
- Waist circumference - 35 inches or over (in women) or 40 inches or over (in men)
- Waist-to-hip ratio - 0.96 – 1.0 for men or 0.81 to 0.85 for women (moderate risk) or 1.1 for men or 0.86 or higher for women (high risk)
- High blood pressure – blood pressure higher than 140/90
- Abnormal cholesterol or triglyceride profile - triglycerides over 150, LDL over 130 (less than 100 is ideal), VLDL less than 10 and HDL under 50 (60 or over is ideal). Triglyceride/HDL ratio greater than four and total cholesterol/HDL ratio greater than 3 are also risk factors.
- History of gestational diabetes or having given birth to a baby over 9 pounds
- Close family members with history of type 2 diabetes, high blood pressure or arteriosclerosis
- Older age – aging allows for more free radical damage to cells and can increase the risk of insulin resistance, especially after the age of 45.
- Asian, Hispanic, African American, Native American or Middle Eastern ethnicity.
- Leading a sedentary life with little or no exercise – inactivity and insulin resistance goes hand-in-hand as muscles use glucose more than any other tissue. When muscles are not active, they are not burning off stored glucose for energy and lowering levels by refilling their reserves with glucose taken from the bloodstream. Inactivity makes muscles less sensitive to insulin.
- Eating excess amounts of simple carbohydrates
- Insufficient sleep – people who sleep five hours or fewer are two and a half times more likely to develop insulin resistance.
- Chronic Stress - Constant production of cortisol keeps blood sugar elevated too long, which triggers overproduction of insulin from the pancreas.
- Steroid use – steroids given to combat inflammation mimics cortisol, which causes blood glucose levels to rise and remain elevated.
How Genes Factor Into the Equation
Although insulin resistance and type 2 diabetes can be caused and reversed by measures related to diet  and lifestyle, an individual’s unique genetic makeup can be a significant contributing factor. Some fortunate individuals possess a greater insulin threshold that enables them to handle carbohydrates. However, about a fourth of the population cannot process very much sugar and starch in their diets without producing excessive insulin. Should these people eat the typical modern diet, their pancreas would have to produce five to six times the normal amount of insulin to lower blood glucose levels. In people over 50, the number insensitive to insulin doubles and is as high as 85% in overweight individuals. If a person’s reserve of insulin-secreting pancreas cells is small, even people who only carry ten to twenty extra pounds can easily become diabetic.
and lifestyle, an individual’s unique genetic makeup can be a significant contributing factor. Some fortunate individuals possess a greater insulin threshold that enables them to handle carbohydrates. However, about a fourth of the population cannot process very much sugar and starch in their diets without producing excessive insulin. Should these people eat the typical modern diet, their pancreas would have to produce five to six times the normal amount of insulin to lower blood glucose levels. In people over 50, the number insensitive to insulin doubles and is as high as 85% in overweight individuals. If a person’s reserve of insulin-secreting pancreas cells is small, even people who only carry ten to twenty extra pounds can easily become diabetic.
A family history of diabetes or other blood sugar imbalances is obviously a significant risk factor along with any history of obesity, early heart disease, dementia or cancer. However, be assured that genetic propensity does not doom you to develop a condition or disease. It is a matter or whether or not the switches that activate genes get turned on by diet, stress and various environmental factors. It has been said “genetics loads the gun, but environment pulls the trigger”. You can keep the trigger from going off with the right healthy diet and lifestyle choices.
Special Note - If you suspect that you may have insulin resistance or pre-diabetes, I have listed at the conclusion of this article the blood tests that are most recommended for helping you to learn your true risk early on while there is still time to take appropriate measures to correct blood sugar imbalances and prevent the development of type 2 diabetes or any associated health problems.
What You Can Do to Reverse Insulin Resistance
A number of steps can be taken to reverse insulin resistance and increase sensitivity of cells to the  action of insulin. For the purposes of this article, I will just highlight briefly some of the most important ones. For more thorough information and guidelines, I would recommend Dr. Mark Hyman’s book “The Blood Sugar Solution”, which you will find an excellent resource that covers the gamut concerning reversing insulin resistance, pre-diabetes, type 2 diabetes, obesity and associated conditions.
action of insulin. For the purposes of this article, I will just highlight briefly some of the most important ones. For more thorough information and guidelines, I would recommend Dr. Mark Hyman’s book “The Blood Sugar Solution”, which you will find an excellent resource that covers the gamut concerning reversing insulin resistance, pre-diabetes, type 2 diabetes, obesity and associated conditions.
Eat to Control Blood Sugar Levels
Dietary measures are the most effective way to maintain tight control on your blood sugar levels and help your cells become more sensitive to insulin. Eating the right balance of carbohydrates, protein and fats for your type of metabolism and focusing on quality, unprocessed nutrient-dense foods in their whole form is the primary way to reverse any imbalance in the body. Eating at regular intervals, spaced apart by at least three hours, and avoiding eating within three hours of bedtime are also effective ways to regulate blood sugar and insulin levels.
- Carbohydrates – Since the body has a limited capacity to store excess carbohydrates, you can help reverse insulin resistance, balance your blood sugar and restore normal insulin metabolism by reducing carbohydrate consumption and increasing lean protein sources and good fats. It is not just the amount of carbs but the type and quality of carbs that will make the difference. Refined, processed (anything containing flour) starchy vegetables, higher glycemic fruits and most grains (modern grains contain high amounts of the type of starch that quickly breaks down to sugar) should be eliminated and replaced with nutrient-dense whole foods, especially colorful fresh fruits and vegetables with an emphasis on non-starchy vegetables (an
 d lots of them!), lower glycemic fruits and legumes, nuts, seeds and beans.For more information on choosing the right types of carbohydrates, I would refer you to my article “The Type of Carb Matters”.
d lots of them!), lower glycemic fruits and legumes, nuts, seeds and beans.For more information on choosing the right types of carbohydrates, I would refer you to my article “The Type of Carb Matters”. - Protein – Protein not only does not raise blood sugar but it increases satiety, reduces appetite, boosts metabolic rate, helps maintain muscle (the best tissue for burning sugar, carbs and fats) and, best of all, triggers the release of glucagon that causes the body to burn fat and block insulin’s efforts to convert blood sugar to fat. Starting your day with a breakfast high in protein and eating protein with every meal and snack can go a longs ways in stabilizing your blood sugar. For more information on the benefits and best types of protein, check out my article “Powered by Protein”.
- Fats – The right balance of fats is especially important for reversing insulin resistance. Healthy fats have anti-inflammatory and antioxidant properties shown to protect against insulin resistance. Transfats and too many of the wrong type of saturated fats in the diet, along with deficiencies in dietary and/or supplemental Omega-3 fats, stiffen cell membranes and cause them to lack the fluidity and flexibility they need to respond to insulin and absorb glucose. Especially avoid anything that contains hydrogenated or partially hydrogenated oils, margarine, or processed oils (such as soy, corn, safflower, sunflower, peanut, and canola). Instead use healthier oils such as extra virgin olive oil, coconut oil, organic butter or ghee, flaxseed oil (never heated), and unrefined cold-pressed oils such as avocado, walnut, grapeseed, almond, hazelnut or hempseed oils. For more information on how to eat the right balance of fats and the type of fats that are most anti-inflammatory and beneficial to the body, I would encourage you to read my article “True Facts on Fats”.
Lose Weight
Losing just 5 to 7 percent of body weight prevents or delays diabetes by 60 percent, according to the Diabetes Prevention Program (DPP), a major multicenter research study. The most effective way to lose weight is to keep your body from overproducing insulin by controlling blood sugar. If sugar and insulin levels are high, then fat is stored and not used. Only when carbohydrates are reduced can fat be mobilized. If you eat food that spikes your insulin level, you will gain weight. If you eat food that reduces your insulin level, you will lose weight.
Exercise
 Exercise is critical for improving sensitivity since it helps keep glucose levels in balance by causing cells to demand more energy. The more muscle a body has, the more glucose it can burn to control blood glucose levels. Due to the number of insulin receptors on the muscle cell, muscles that are conditioned are more responsive to insulin and blood sugar than non-conditioned ones. Exercise can enable glucose to enter muscle cells even when insulin is not present.
Exercise is critical for improving sensitivity since it helps keep glucose levels in balance by causing cells to demand more energy. The more muscle a body has, the more glucose it can burn to control blood glucose levels. Due to the number of insulin receptors on the muscle cell, muscles that are conditioned are more responsive to insulin and blood sugar than non-conditioned ones. Exercise can enable glucose to enter muscle cells even when insulin is not present.
According to a study published in the Journal of Clinical Endocrinology and Metabolism, just one hour of exercise per day for one week starts to increase beta-cell function and insulin sensitivity. Walking 30 minutes a day is recommended though more vigorous and sustained exercise is often needed to reverse severe insulin resistance or diabetes. Strength training and interval training work in different ways to help overall blood sugar balance and energy metabolism by building and maintaining muscle and increasing the efficiency of calorie burning.
Use Supplements That Improve Insulin Sensitivity and Glucose Metabolism
Omega-3 fish oil, magnesium, chromium, vanadium, antioxidants like vitamin C and E, alpha-lipoic acid (very effective for reducing blood sugar and reversing blood sugar-caused nerve damage or neuropathy), cinnamon, herbs (bitter melon, gymnema, banaba leaf, fenugreek are among the most noted to help regulate blood sugar) and extra fiber. Some formulas that I recommend that are designed to balance blood sugar levels and support the pancreas are SugarReg, GTF Chromium, Target P-14 and Alpha Lipoic Acid.
Concluding Thoughts
Controlling blood sugar to control insulin levels is a powerful way to enjoy greater health and energy, maintain a fit body weight and spare yourself the health consequences that await downstream from imbalanced blood sugar levels. Control your blood sugar….control your health. You will be glad that you did.
Sources:
The Blood Sugar Solution – by Mark Hyman, MD
Reversing Diabetes – by Julian Whitaker, MD
Stop Prediabetes Now – by Jack Challem
The End of Diabetes by Joel Fuhrman, MD
Diabetes without Drugs – Suzy Cohen, RPh
Life without Bread – by Christian B. Allan, PhD & Wolfgang Lutz, MD
It Starts with Food – by Dallas and Melissa Hartwig
RECOMMENDED MEDICAL TESTING
Several of these tests are not ordered on a conventional basis unless a person’s blood sugar is already significantly elevated. However, more progressive, prevention-oriented doctors recommend them as a valuable means of evaluating blood-sugar/insulin imbalances earlier on in the continuum that culminates in Type 2 diabetes. In other words, they can clarify your risk and help access if you are already insulin resistance and/or pre-diabetic. You may order these tests yourself online if you are not able to get them through your doctor.
The first three tests includes “better” and “best” ranges in addition to the normal ranges that were taken from Jack Challem’s book “Stop Pre-Diabetes Now”.
Fasting Glucose – this conventionally ordered test gives a snapshot of your glucose levels from a sample  of blood taken in the morning before you eat or drink anything except water.
of blood taken in the morning before you eat or drink anything except water.
- Normal range - 65-99 mg/dl
- “Better” range – 75-85 mg/dl
- “Best” range – 80-82 mg/dl
Fasting Insulin – since insulin levels often become too high many years before blood sugar levels rise, this test helps to show how hard insulin is having to work to get glucose into your cells – a much greater predictor of the potential development of pre-diabetes or type 2 diabetes.
- Normal range – 6-35 mcIU/ml
- “Better” range – less than 10 mcIU/ml
- “Best” range – less than 7mcIU/ml
- Pre-diabetic range – more than 11mcIU/ml
Hemoglobin A1c – this test measures glycated hemoglobin (the degree to which glucose has bound to hemoglobin, a substance in red blood cells) and provides a way to determine a blood sugar average over a two to three month period.
- Normal – 4.5-5.7%
- “Best” – less than 5%
- Pre-diabetic – 5.7-6.9%
- Diabetic – 7% or higher
Oral Glucose Tolerance Test (OGTT) – this test involves a series of glucose measurements after you drink a sweet liquid beverage that contains glucose. Repeated blood samples are taken over the course of 1 hour, or sometimes 2 hours. The test tracks how well you tolerate glucose and how you process the glucose after consuming it. Here are the normal ranges based on 75 grams of glucose:
- After 1 hour – less than 200 mg/dl
- After 2 hours – less than 140 mg/dl
Insulin Response Test – this test measures fasting, 1-hour, and 2-hour glucose and insulin levels after 75-gram glucose load. It is like the glucose tolerance test but measures both glucose and insulin. Dr. Mark Hyman, author of “The Blood Sugar Solution” gives the following parameters for test interpretation:
- Fasting insulin - should be less than 5 IU/dl
- 1- and 2-hour insulin levels – should be less than 30 IU/dl.
- Fasting blood sugar - should be less than 90 mg/dl
- 1- and 2-hour blood sugar – should be less than 120 mg/dl
Copyright © 2008-2015 Lucinda Bedogne, CNHP, CNC
Post Your Comment...
|
|
||||||||||||


